The narrative was straightforward, seductive—science had finally cracked the code. But what if the science behind Ozempic was wrong? Not fraudulent, but critically oversimplified, leading to inflated expectations, overlooked risks, and a fundamental misunderstanding of how this powerful drug truly works?
Table of Contents
For years, headlines screamed miracle: Ozempic, the diabetes drug turned weight-loss phenomenon, promised to revolutionise obesity treatment. Celebrities flaunted dramatic transformations. Doctors prescribed it off-label at unprecedented rates.
Buckle up—hstech.io is diving deep into the evolving, complex reality of GLP-1 agonists like Ozempic.
What is Ozempic? The Foundation
Ozempic is the brand name for semaglutide, a GLP-1 (glucagon-like peptide-1) receptor agonist. Developed by Novo Nordisk, its primary FDA approval is for managing type 2 diabetes:
- How it works (initially thought): Mimics the GLP-1 hormone, stimulating insulin release when blood sugar rises, suppressing glucagon (which raises blood sugar), and slowing gastric emptying. This leads to better blood glucose control.
- The Weight Loss Bonus: During trials, a significant side effect emerged: substantial weight loss. This led to the higher-dose version, Wegovy, which was explicitly approved for chronic weight management.
The initial scientific narrative was compellingly straightforward: Ozempic reduces appetite and slows digestion → you eat less → you lose weight and control blood sugar.
Simple. Marketable. Effective… but incomplete.
Why the Alarm Bells? “The Science Behind Ozempic Was Wrong”, Explained
The claim “the science behind Ozempic was wrong” doesn’t mean the drug is ineffective or unsafe for its approved uses. Instead, it highlights how the early understanding and communication of its mechanisms and long-term implications were oversimplified, incomplete, or prematurely conclusive. Here’s where the initial picture fell short:
1. Oversimplified Mechanism: Beyond Just Appetite & Digestion
- The Early Story: “Ozempic makes you feel full faster and longer. Less food in = weight loss.” This focused almost exclusively on peripheral effects (stomach, digestion).
- The Emerging Complexity: Research now reveals Ozempic works through a complex orchestra of systems:
- Brain Reward Pathways: Semaglutide directly impacts the hypothalamus (appetite control) and mesolimbic pathways (reward, craving, motivation). It reduces the “reward value” of high-fat, high-sugar foods, fundamentally changing desire, not just hunger.
- Gut-Brain Axis Signalling: It modulates intricate communication between the gut microbiome, gut hormones, and the brain, influencing satiety, inflammation, and metabolic health far beyond simple fullness.
- Fat Metabolism Regulation: Evidence suggests that GLP-1 agonists may alter the function of fat cells (adipocytes), potentially improving fat storage efficiency and energy utilisation.
- Hormonal Cascade Effects: The impacts extend to other hormones, such as leptin, ghrelin, and peptide YY, creating a complex feedback loop.
- Why it Matters: Viewing Ozempic solely as an appetite suppressant grossly underestimates its profound neurological and metabolic effects. This complexity explains variability in individual responses and hints at potential broader applications (and risks).
2. The Weight Loss Permanence Myth: The Rebound Reality
- The Early Implication: Marketing and initial enthusiasm often suggested that the weight loss achieved with Ozempic/Wegovy could be maintained relatively easily in the long term.
- The Hard Data: Landmark studies, such as the STEP 1 extension and real-world evidence, paint a different picture. When patients stop taking semaglutide:
- Significant weight regain occurs: Typically, approximately two-thirds of the lost weight returns within one year.
- Metabolic benefits reverse: Improvements in blood sugar, blood pressure, and cholesterol often diminish over time.
- Why it Matters: This demonstrates that Ozempic manages the biological drivers of obesity while the individual is active; it doesn’t cure them. The science initially underestimated the body’s powerful homeostatic mechanisms, which helped pull the weight back up. Long-term (potentially lifelong) therapy is likely necessary for sustained results, raising questions about cost, access, and decades-long medication use.
3. Metabolic Assumptions: More Than Just Glucose and Appetite
- The Early Focus: Benefits were primarily attributed to weight loss itself and direct effects on blood sugar/appetite pathways.
- The Broader Impact: Ozempic exhibits effects independent of weight loss:
- Cardiovascular Protection: Semaglutide significantly reduces the risk of major cardiovascular events (heart attack, stroke) in people with type 2 diabetes and established heart disease (SUSTAIN-6, SELECT trials). This is partly due to its anti-inflammatory and direct cardioprotective effects.
- Anti-Inflammatory Actions: GLP-1 RAs reduce systemic inflammation markers, such as C-reactive protein (CRP), potentially benefiting conditions like non-alcoholic steatohepatitis (NASH) and atherosclerosis.
- Neuroendocrine Effects: The potential protective effects on brain health (studied in Alzheimer’s/Parkinson’s diseases) and kidney function are being explored.
- Why it Matters: The initial science focused narrowly on diabetes and weight, overlooking potentially profound systemic benefits. Conversely, it also means the risks extend beyond initial assumptions.
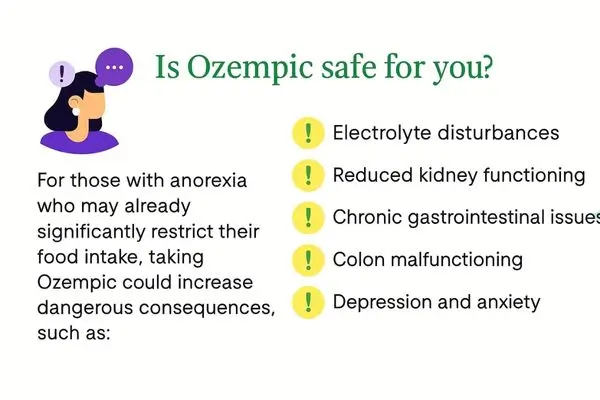
4. Side Effects & Risks: Beyond the Trial Bubble
The Early Safety Profile: Clinical trials focused on common, relatively short-term issues: nausea, vomiting, diarrhoea, and constipation. These were deemed “tolerable” and often transient.
The Real-World Unmasking: Wider, longer-term use reveals a more complex risk landscape:
- GI Distress: Can be severe and persistent (gastroparesis-like symptoms), leading to hospitalisation for some.
- Muscle Mass Loss: A significant portion of weight lost is lean muscle mass, raising concerns about sarcopenia, reduced metabolic rate, and frailty, especially in older adults. Prioritising protein intake and resistance training is crucial.
- Nutrient Deficiencies: Slowed digestion can impair absorption of essential nutrients (vitamins, minerals).
- “Ozempic Face/Butt”: Rapid weight loss can lead to sagging skin/facial volume loss, underscoring the importance of holistic care.
- Gallbladder Disease: Increased incidence reported.
- Pancreatitis & Thyroid C-Cell Tumour Risk: Known risks requiring monitoring (especially with personal/family history).
- Long-Term Dependency Concerns: The weight regain data fuel questions about physiological dependency and the ethics of indefinite treatment.
- Why it Matters: The original science, based on controlled trials of 1-2 years, couldn’t fully predict the spectrum or severity of side effects emerging in millions of diverse users over longer durations. This necessitates ongoing vigilance and patient education.
5. Public Messaging vs. Actual Science: The Simplification Trap
- The Hype: “Inject and lose weight!” Media and (sometimes) marketing reduced the complex pathophysiology of obesity and the drug’s action to a simple equation. Celebrities amplified a “quick fix” narrative.
- The Scientific Reality: Obesity and type 2 diabetes are chronic, complex biopsychosocial diseases driven by:
- Genetics and Epigenetics
- Hormonal Dysregulation
- Neurobiology (Reward Pathways, Stress Response)
- Environmental Factors (Food Access, Marketing, Stress)
- Psychological Factors (Emotional Eating, Trauma)
- Social Determinants of Health
- Why it Matters: Framing Ozempic as a standalone solution ignores the multifaceted nature of these conditions. Sustainable health requires a holistic approach: nutritional therapy, regular physical activity, behavioural support, stress management, and addressing social/economic barriers. Ozempic is a powerful tool, not a magic bullet.
The Corrected Picture: What We Now Understand About Ozempic Now
The evolving science reveals Ozempic as a multifaceted metabolic modulator, not just an appetite suppressant. It works through:
- Central Nervous System Effects: Suppressing appetite and dampening food cravings/reward signals in the brain.
- Peripheral Effects: Slowing gastric emptying, improving insulin sensitivity, and enhancing insulin secretion.
- Systemic Effects: Reducing inflammation, potentially protecting the heart and kidneys, and influencing fat metabolism.
- A Chronic Disease Management Tool: Providing significant benefits while active, but not resetting the body’s underlying weight regulation set point permanently.
Implications: What This Means for Patients and Doctors
- For Patients: Set Realistic Expectations: Weight loss is significant but not always effortless; side effects can occur; stopping usually means regaining weight. This is management, not a cure.
- Prioritise Lifestyle: Use Ozempic in conjunction with a balanced diet, regular exercise, and behavioural changes. Focus on protein intake and strength training to maintain muscle mass.
- Monitor Closely: Report persistent GI issues, significant muscle loss, or other concerns to your doctor. Regular blood work may be needed.
- Think Long-Term: Discuss the plan for potentially years or decades of use with your provider, considering the cost, access, and monitoring requirements.
- For Doctors: Comprehensive Patient Selection & Education: Screen carefully, discuss realistic outcomes, emphasise the necessity of lifestyle integration, and transparently explain risks and the likelihood of long-term use.
- Holistic Treatment Plans: Prescribe Ozempic as part of a comprehensive plan that includes nutritional counselling, exercise guidance, and behavioural health support.
- Vigilant Monitoring: Watch for muscle loss, nutritional deficiencies, gallbladder issues, and psychological impacts. Manage GI side effects proactively.
- Stay Updated: The science is rapidly evolving. Stay informed about new data on long-term effects, emerging risks, and potential new indications.
The Future of GLP-1 Agonists: Beyond Ozempic
The “Ozempic was wrong” narrative is ultimately a story of scientific progress. Research is accelerating:
- Next-Gen Agonists: Tirzepatide (Mounjaro/Zepbound) targets both GLP-1 and GIP receptors, showing even greater efficacy. Triple-agonists are in development.
- Oral Formulations: Making treatment more accessible (e.g., Rybelsus).
- Understanding Mechanisms: Deeper research into brain pathways, gut microbiome interactions, and fat cell biology.
- Broader Applications: Exploring use in NASH, heart failure (HFpEF), addiction, Alzheimer’s, and more.
- Mitigating Side Effects: Researching combinations or formulations to reduce gastrointestinal issues and muscle loss.
- Long-Term Safety Data: Critical studies tracking outcomes over 5, 10, 15+ years are underway.
Conclusion: Science Evolves – Embracing Complexity
The claim “the science behind Ozempic was wrong” isn’t an indictment of the drug’s value. It’s a recognition that early models were incomplete. Ozempic (semaglutide) is a remarkable scientific achievement offering life-changing benefits for many with type 2 diabetes and obesity. However, its story underscores a vital truth in medicine: complex diseases rarely have simple solutions.
The initial narrative of effortless, permanent weight loss through appetite suppression was a dangerous oversimplification. The reality is richer, more nuanced, and still unfolding.
Ozempic works through sophisticated interactions between our gut, brain, metabolism, and hormones. Its benefits are profound but often require ongoing use. Its risks are broader than first thought.
Moving forward, embracing this complexity is key. Patients deserve realistic expectations and holistic support. Doctors need to integrate powerful pharmacological tools, such as Ozempic, into comprehensive care plans.
Science must continue its diligent work, refining understanding and developing even better solutions. The journey of understanding Ozempic isn’t over; it serves as a powerful reminder that science, like human health itself, is a dynamic process of discovery and adaptation.
The miracle isn’t in a single injection; it’s in the relentless pursuit of understanding our bodies and finding better ways to heal. If you want to study helpful guide about weight loss this plan would be helpful for you.
Best Free AI Room Design Tools 2025: Ultimate Guide to AI Interior Design
Pingback: Plated Skin Science Review: Exosome Technology & Top 5 Serum Revealed - HS Tech